Vocal Feminization Surgery Q&A with Dr. Brandon Baird | Wendler Glottoplasty
In the journey of vocal feminization, some individuals may reach a point where they consider surgical options to further align their voice with their gender identity.
One of the most popular surgeries for this purpose is the Wendler Glottoplasty, a procedure that can have significant impacts on vocal pitch and resonance. However, vocal feminization surgery is a complex decision that should be approached with careful consideration and guidance.
Today, I’m thrilled to share an insightful conversation with Dr. Brandon Baird, a leading expert in gender-affirming voice care, Assistant Professor of Laryngeal Surgery at University of Chicago, and the Co-Director of the Voice Center.
In this interview, Dr. Baird explains the process, risks, and potential outcomes of vocal feminization surgery, and why voice therapy should always be part of the conversation.
Enjoy!
Olivia Flanigan: Thank you so much for joining us today for this conversation with Dr. Brandon Baird who is the Assistant Professor of Laryngeal Surgery at University of Chicago and the Co-Director of the Voice Center there. And I am just super excited to speak with you today, Dr. Baird. Thank you so much for being here with me.
Dr. Brandon Baird: Thank you so much for having me, Olivia.
Olivia Flanigan: So I want to ask you some questions just about yourself, a little bit about your background, and how you've gotten into voice and this Wendler Glottoplasty procedure specifically.
Dr. Brandon Baird: Yeah, sure thing. So I did a four-year med school. And after the end of med school, or as I was approaching the end of med school, I thought about what I wanted to do. I thought about doing something that was surgical. And I have a background in singing. And so that led me to otolaryngology, or ENT, as a subspecialty to do my residency in. I did five years of residency at Stanford. And then towards the end of that, I really, again, sort of resonated with the patients that had voice disorders and were singers and performers, teachers. They really resonated with me. So I decided to go down that route.
And then I was really lucky to find that there is an entire subpopulation of patients to be able to take care of that were gender affirming patients after sort of finishing my fellowship in laryngeal surgery. And that was something that really sort of resonated with me and just was really rewarding, a great patient population to take care of.
Olivia Flanigan: Amazing. It's wonderful that you can kind of bridge that gap in your singing life and your doctor life. So, tell me a little bit about what it's like when a patient comes into your care at the University of Chicago.
Dr. Brandon Baird: Yeah, we have a wonderful, wonderful program at the University of Chicago. It's a trans care gender affirming program that really allows us to connect with the patients from a multidimensional standpoint. We have OB providers and primary care providers that help patients get set up with hormones. We also have providers that are plastic surgeons that help with top and facial feminization surgery. We also have providers and surgeons that are urologic surgeons. And so we offer kind of a complete array of gender affirming care. My kind of area of expertise is gender affirming voice care and also tracheal shave.
And so initially a lot of patients will come in to see both me and a speech pathologist that I work with. Her name is Dana Hayes. She's excellent. And they'll kind of do a consultation with both of us where we ask them about what some of their goals are from a vocal standpoint. We evaluate both not only their physical exam, but also their voice box to make sure that there's no underlying abnormality that would potentially preclude them or make it difficult for us to do some of these surgeries. And then we talk to them about some of the options, both surgical and also therapeutic, like voice therapy that might be available for them for gender affirming voice care.
Olivia Flanigan: OK, wonderful. So can you tell me just just briefly what kinds of things that you would look for for a patient who was not a good candidate for a surgical option, for example, or something that might be problematic during therapeutic care?
Dr. Brandon Baird: Yeah, I think that there's a huge, really sort of an importance of emphasis that has to be made on both anatomic abnormalities that might preclude doing a surgery. For instance, if the patient has a significant scar on their vocal cords that might make subsequent surgery, voice surgery difficult and or make their outcome a lot worse. So we might counsel them. Maybe we consider doing more of a therapeutic or voice therapy tract rather than sort of going towards a surgery route.
Patients that have any underlying malignancy or cancer certainly would be out because we'd want to address sort of the underlying medical issue first before sort of going to gender affirming kind of strategy. Additionally, from a patient expectation standpoint, there's a lot of work that has to be done in terms of making sure that the provider meets the patient where they are and talks about expectations, talks about potential outcomes.
A lot of patients, as you know, and as many of you know, have dysphoria with even the idea or concept of hearing their own voice. That's really a hurdle that they have to be able to overcome to be able to be successful in certain circumstances, especially as it relates to some of the post-operative therapy that we provide.
Really a lot of modifications, a lot of voice therapy involves experiencing and sort of engaging with the sound of your voice and making modifications based on what you hear. So we really have to have, make sure that patients are able to at least engage in that process. And it's one of the big reasons why I send patients, all my patients to voice therapy first. And of the patients that do voice therapy, about 95% of them find that the voice therapy is actually sufficient to get them the kind of sound, the quality of sound and also sort of the presentation that they're hoping for, that they're looking for.
Olivia Flanigan: That's wonderful. So if a patient were to come and say, I know for sure that I'm ready for surgery, would you still encourage them to go through the therapy?
Dr. Brandon Baird: I would, especially if they haven't done it before. There are a lot of patients that see me that have done therapy before, and usually we give them a little bit of an abbreviated tract. We want to make sure that we have some preoperative voice measures. We want to make sure that the experiences that they've had are sort of similar to what our speech program provides. But if a patient's coming into Novo who hasn't necessarily had any exposure to voice therapy, I tend to really want them to sort of give the voice therapy the full understanding full college try before we start to talk about surgical options.
I always talk about the fact that any procedure that I do, any invasive procedure comes along with risks. If there's something that we can do to get you to where you need to be that is non-invasive, that's always my preference, as opposed to doing things that potentially can cause harm, that potentially can cause you know detrimental voice outcomes. And so we talk about those in depth as well.
Olivia Flanigan: Amazing. Can you tell us just a little bit about the procedure that you do, the Wendler Glottoplasty.
Dr. Brandon Baird: Yeah. So there are actually a number of different procedures, as many of you know, that can be used to help address the voice and sort of help to affirm the voice, I should say. The first procedure that I'm aware of that was described was actually back in the 90s, I want to say, or 80s. It was the law that's a laser-assisted, basically vocal cord thinning that basically uses the laser to scar the superior aspect of the vocal cords that sort of shrinks them a little bit. That sort of fell out of favor for the Wendler Glottoplasty, which came along in the late 90s and early 2000s. That's what most of the laryngologists or laryngeal surgeons, what most of us engage in. That involves creating a web, basically a scar between the two vocal cords.
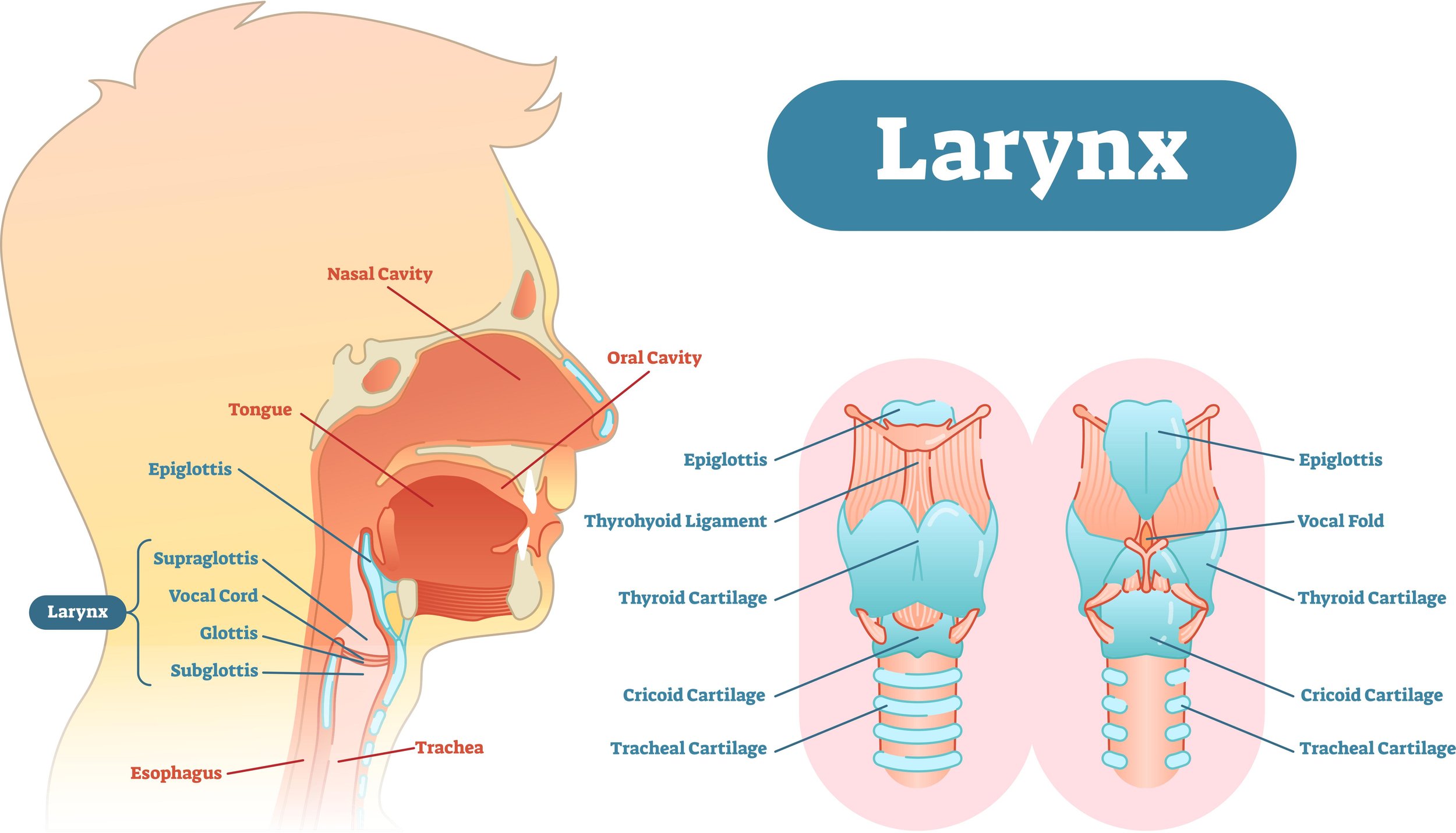
Our vocal cords are composed of sort of small structures that are in the shape of a “V” that sit right here at the area where sort of, our thyroid cartilage or Adam's apple is. They open up when we breathe in. They close when we speak, swallow, and sing. And air comes up from our lungs and vibrates those vocal cords and makes sound. There are three different things that can address the pitch of the voice. The first thing is the size of the vocal cords, the size and the density of the vocal cords. The next thing is the length of the vocal cords. And the last thing is the tension on the vocal cords. Addressing all three of these things can potentially address or change the voice.
The Wendler Glottoplasty addresses the pitch by shortening the vocal cords. So rather than starting here, it kind of creates a scar between the two sides and creates a shorter vocal cord. What that does is it increases not only the pitch, or increases the fundamental frequency is what we call it, but it also can have other sort of consequences like decreasing the amount of air pressure and sound pressure that comes through the voice box. That can oftentimes cause patients to be quite much more quiet postoperatively than they were beforehand.
So the Wendler is a great option. It's tried and true. It's kind of tested. It's kind of the workhorse. Now, there are a lot of other options that have been evolved or that have evolved over the past five years or so. One of the options that I'm actually doing more of now is the retro displacement of the anterior commissure and vocal fold shortening, or the VFSRAC. That is a procedure that was initially created in South Korea by the Yeson Institute, which does something very similar to the Wendler, but it does a little bit of a better job of creating that kind of cone of airflow through the vocal cords. So patients tend to have a little bit of a better outcome according to the Yeson Institute with that surgery.
And then lastly, there is an option to do something called a feminization laryngoplasty, which is basically an external approach where the entire larynx is sort of deconstructed and reconstructed to not only shorten the vocal cords, but also to stretch them and sort of create a little bit more tension that allows for patients to develop a really kind of higher pitched voice. That's nice.
Olivia Flanigan: Wow. OK, I didn't know about that one. So, with that, is that a more involved recovery?
Dr. Brandon Baird: It is. So, it's a little bit of a riskier surgery and it's a more involved recovery. As far as I know, there's only one person in the country that does that surgery. There may be others that have started to sort of take it on as some of his fellows. But there's only one person in Oregon that does that type of surgery.
Olivia Flanigan: Okay. Now, can you tell me a little bit about the results and generally how happy people are with the results? How much higher is the voice, et cetera?
Dr. Brandon Baird: Yeah. So the results can vary from patient to patient. But in general, what's been reported in the literature is that you can get anywhere from, hertz being the frequency of the pitch, so someone that has a male register is between 100 and about 150, 180. A female register is over 200 or 250. And then there's a sort of gender neutral range between 150 and, say, 210 or so. So typically, if you think about that as sort of a scale, typically something like a Wendler can get a patient anywhere from 50 to 150 Hertz higher than where they were before. But that's variable. It depends on the patient. It depends on how much work is put in both before and also after surgery. And I really stress this point that, you know, the results are not necessarily guaranteed, so to speak, and that there's a lot of work that has to go into, you know, making the voice sound the way that we want it to sound.
Olivia Flanigan: And so what is the recovery period like?
Dr. Brandon Baird: Yeah. So typically the surgery is an endoscopic surgery. It's all done through your mouth, basically. After the surgery, we'd put patients on a period of voice rest for three weeks, at least I do. I did that intentionally because we are suturing endoscopically. We're placing sutures under a very, very small, under a microscope in a very small area.
And we wanna make sure that those sutures stay put where we've placed them. We don't want the vocal cords to rip open and then create potentially a scar between the two sides. So I put patients on voice rest for about three weeks. At the three-week mark, I started letting patients use their voice a little bit more. And what that does is actually allows the patients to start kind of learning this new instrument that they have.
I always tell patients it's gonna be about three months or so of having a pretty bad or what we call dysphonic voice. And a lot of patients are very hoarse or they have trouble sort of figuring out where to place their voice after the surgery. The Yeson Institute actually sometimes will use Botox to help prevent the patients from sort of working too hard and sort of stressing that suturing that's performed.
So, it is a long, slow journey after the first, after that surgery. So it sometimes takes, like I said before, months until patients get to where they sort of think that they have, you know, they feel like they have a good voice. In addition to that, any small complication along the way, granulation tissue, which is basically like a scab that's not really, you know, that doesn't, grows in a poor place or the suture is breaking or any other number of potential complications can extend that period of time even longer.
Olivia Flanigan: Okay. And you mentioned before how you can sort of end up with a very quiet sounding voice. Are there things that patients do in therapy to remediate that?
Dr. Brandon Baird: Yeah, so certainly in therapy, and it's a good question for one of my colleagues. Her name is Dana Hayes. In therapy, there are techniques, and I'm sure Olivia, you do this as well, techniques to help improve breath support, help to improve, you know, general sound pressure, forward focus, resonance, those types of things that can help to address the projection of the voice. But some of them are, all of these interventions are potentially limited by the underlying anatomic issue.
So despite some of the techniques that can be learned through voice therapy, they still may not be able to overcome some of these associated expectations of having acquired a voice. And some patients, especially, you know, a lot of our gender affirming patients here on the south side or in areas that are a little bit less supportive of gender nonconforming people, that can be a real danger. And so we really want to make sure we counsel patients about that beforehand.
Olivia Flanigan: Okay. Can you give me a sense of I mean, obviously, insurance is is a broad topic and different in so many states. But can you give me a sense of maybe what percentage of people are able to use insurance with you specifically?
Dr. Brandon Baird: It's frustrating because it depends not only on the insurance carrier, the patient, the paperwork that's done beforehand, but the institution as well. And there are always so many small little discrepancies that can just make both the patients and also us as providers our life hell. We don't want the patients to have to pay any more than they want. We don't want them to have to pay anything, honestly.
But I think hospital systems are increasingly corporatizing and insurance companies are increasingly not paying for things, I think, especially in the current political climate that we're in. And I think as a result of that, there ends up being this sort of gap in communication and expectation about what patients think that they're paying for prior to the start of a visit and what patients actually get billed for.
And I think it's very important that patients sort of take, try to take as much autonomy in terms of managing that aspect of their financial aspect of that care, calling the call center and asking for the finance department, finding out what the exact out-of-pocket expense would be for their visit, calling their insurance company and asking what the anticipated out-of-pocket expense would be for the specific codes, that are going to be billed for that visit so that there's not that discrepancy.
In terms of answering your question, I'm sorry, I'm getting a little long winded. I'd say that probably about 25% of patients come without insurance. And I'd say that there are probably 10% of patients that come with insurance, but there is a disparity or discrepancy between what the university takes and their insurance, which then leads to issues on the back end. So clarity and communication, lack of ambiguity, trying to be as clear as possible, really helps to avoid some of these really unfortunate things that can happen for our patients who are already under so much stress, just nationally and socially and just in terms of their life.
Olivia Flanigan: It’s such a shame that it needs to be such a wild goose chase to figure out the basic facts when it comes to that, but that's great information to what specifically to ask for and who to ask for. Is there anything else that you would want patients to know coming into this process or coming into vocal surgery? Anything, expectations that you think are important to know about?
Dr. Brandon Baird: Yeah, you know, I think a lot of patients come in hearing about surgery and say, oh, I just want that. And as we mentioned before, I think it's really important to approach therapy with an open mind. I think it's very, very helpful for a lot of people. And nine times out of 10, I will try to really advocate for that as an option.
There are patients where they say, I've really done eight sessions of therapy, I've worked hard, and I'm feeling like I just can't either meet the expectations, or more importantly, I'm feeling fatigued to to be able to sort of, I can't get to where I want to be without feeling major fatigue or discomfort. And oftentimes, if that happens, we start to talk to patients about surgery a little bit more kind of in depth.
It's important to go to a place that acknowledges the role and the importance of voice. So you want to go to a typically a laryngeal surgeon to do some of this work, is ideal or someone that's a laryngologist.
The other thing that you want to be mindful of, and it's something that I've seen a lot when it comes to tracheal shave, I know it's kind of a little off topic, there's a significant risk to the voice after these types of surgeries, specifically tracheal shave. A lot of times they get sort of bundled into facial feminization surgery with a plastic surgeon, and that's wonderful.
But someone needs to look at the cords while the Adam's apple or the thyroid cartilage is being removed, which means that someone has to take a look from above while the surgery is happening to make sure that too much of the Adam's apple is not removed. If that happens, the vocal cords can get loose and it can create a sound of the voice that's actually lower than what the voice was prior to that type of surgery.
So that's a really important kind of message and warning to any sort of gender affirming individuals seeking gender affirming care, because we want to make sure that, you know, people are not going into some of these surgeries and then ending up worse off after the surgery.
Olivia Flanigan: Great, great information. Thank you so much. Well, I think that about does it for my questions for you. So I really, really appreciate your time, Dr. Baird, and your expertise. This has been so great, and I hope this helps some people who are going into this process and have a little bit of information before they step in the door.
Dr. Brandon Baird: Wonderful, wonderful. Happy to help, and please reach out to me if there are any questions. Thank you so much. Bye-bye.
Olivia Flanigan: Bye-bye.
Conclusion
Vocal feminization surgery, such as the Wendler Glottoplasty, can be an excellent option for some individuals seeking to achieve a more feminine voice. However, it's essential to approach this decision with a comprehensive understanding of both the surgical procedure and the accompanying recovery process.
As Dr. Baird emphasizes, voice therapy plays a vital role in achieving the best results, and for many, it can offer the vocal transformation they desire without the need for surgery.
If you're considering vocal feminization surgery, it's important to connect with experienced professionals and have an open conversation about your goals, expectations, and options.
Whether through therapy or surgery, the right path is one that empowers you to find your true voice.